Question: Do you know of a revenue cycle management tool that can automate claim submissions and optimize collections for healthcare providers?

Availity
If you're looking for a full-featured revenue cycle management system to automate claims submission and optimize collections for healthcare providers, Availity is a top pick. Availity's system has a lot of features for the pre-service, post-service and post-adjudication steps of revenue cycle management. It includes automated processes for claims submission, denial avoidance and denial management, as well as AI-based prior authorization and coverage verification. It also has real-time collaboration and digital communication tools, making it a good tool for optimizing collections and improving operational efficiency.
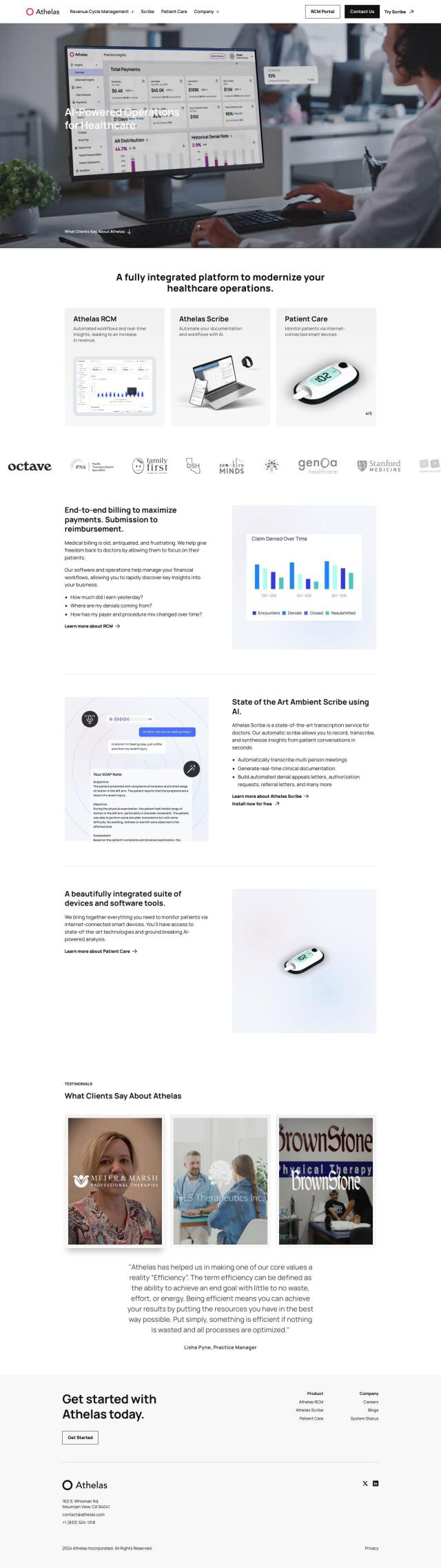
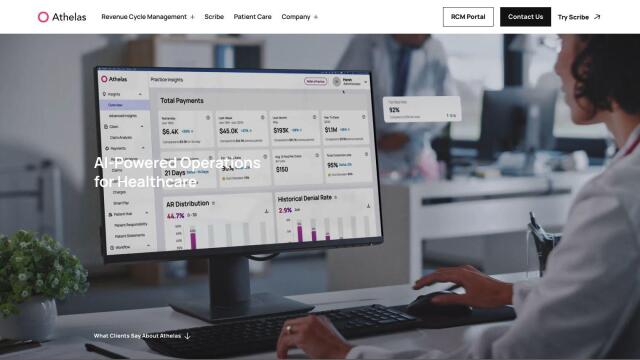
Athelas
Another top pick is Athelas, which uses AI to automate many aspects of healthcare. Athelas RCM offers real-time insights into revenue cycle management and includes same-day claims submission and live reconciliation. It also integrates with more than 20 EHRs, so it's a good option for those who want to increase productivity and improve patient care. Athelas also offers AI-based transcription and automated denial appeals, among other features to automate administrative tasks.

CharmHealth
If you're looking for a broader suite of tools, check out CharmHealth. CharmHealth is a cloud-based system that includes a Meaningful Use Certified EHR system, Practice Management Tools, and a full Revenue Cycle Management system. Automated claim submission, billing and insurance management can help automate the revenue cycle process. The system also supports telehealth solutions and patient engagement platforms, making it a good option for improving performance and reducing costs.
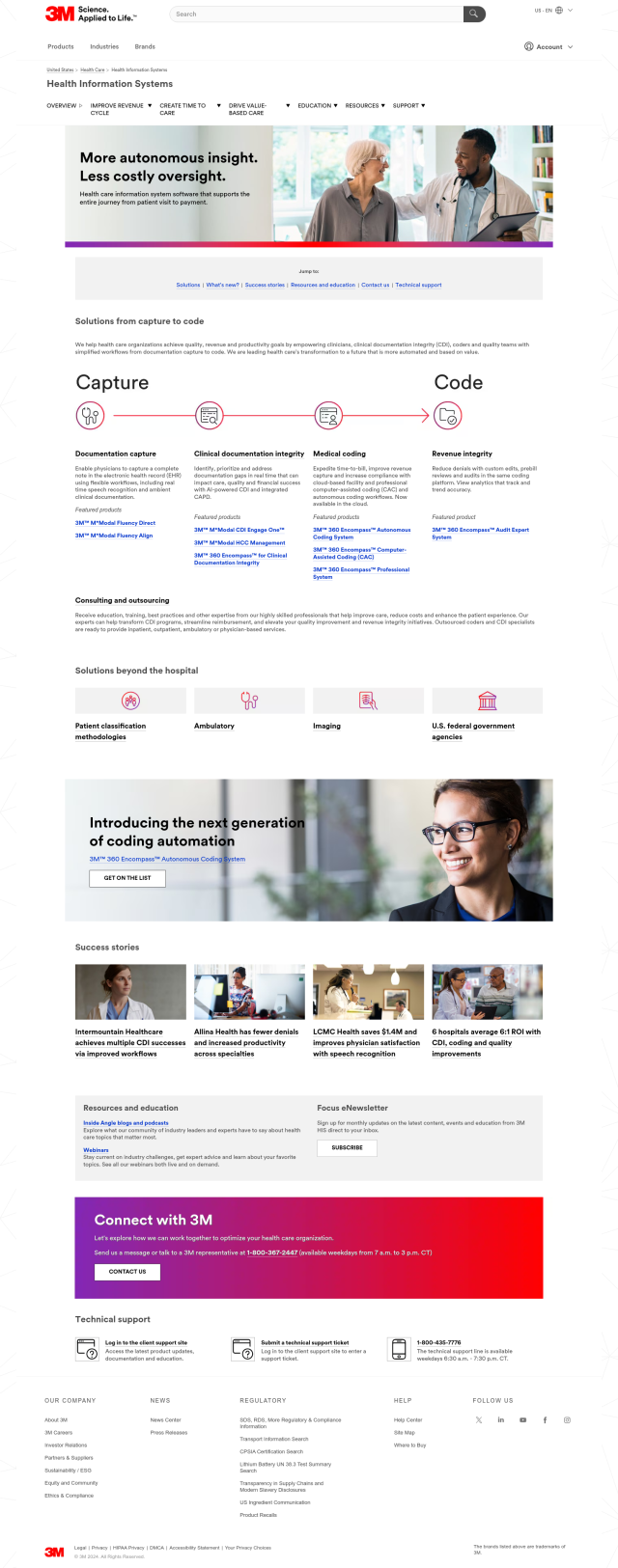
Health Information Systems
Finally, Health Information Systems from 3M offers a variety of tools designed to improve revenue cycle management and physician care. The system includes AI-based CDI, real-time speech recognition and automated coding workflows. With tools like 3M M*Modal Fluency Direct and 3M 360 Encompass Autonomous Coding System, the system is designed to improve healthcare by making it more automated and value-based.