Question: Can you recommend a solution that streamlines the prior authorization process in healthcare, making it more efficient and patient-centered?
Cohere Health
If you need a way to automate the prior authorization process, Cohere Health has a full platform called Cohere Unify designed to streamline prior authorization processes, making them more efficient, accurate and patient centered. It includes tools like Intake for digitizing prior authorization requests, Decisioning for automating decisions based on health plan-preferred policies, and Review for AI-assisted manual review and automated queue management. This can help reduce administrative costs and denial rates, ultimately resulting in better patient care and outcomes.

Availity
Another good option is Availity. Its integrated provider engagement platform streamlines administrative and clinical work for healthcare providers and payers. The platform includes AI-powered prior authorization options, customizable claim submission and status options, and denial prevention and management options. Availity's platform reduces waste and abrasion, helping to improve patient care and drive operational excellence by processing more than 13 billion transactions per year.
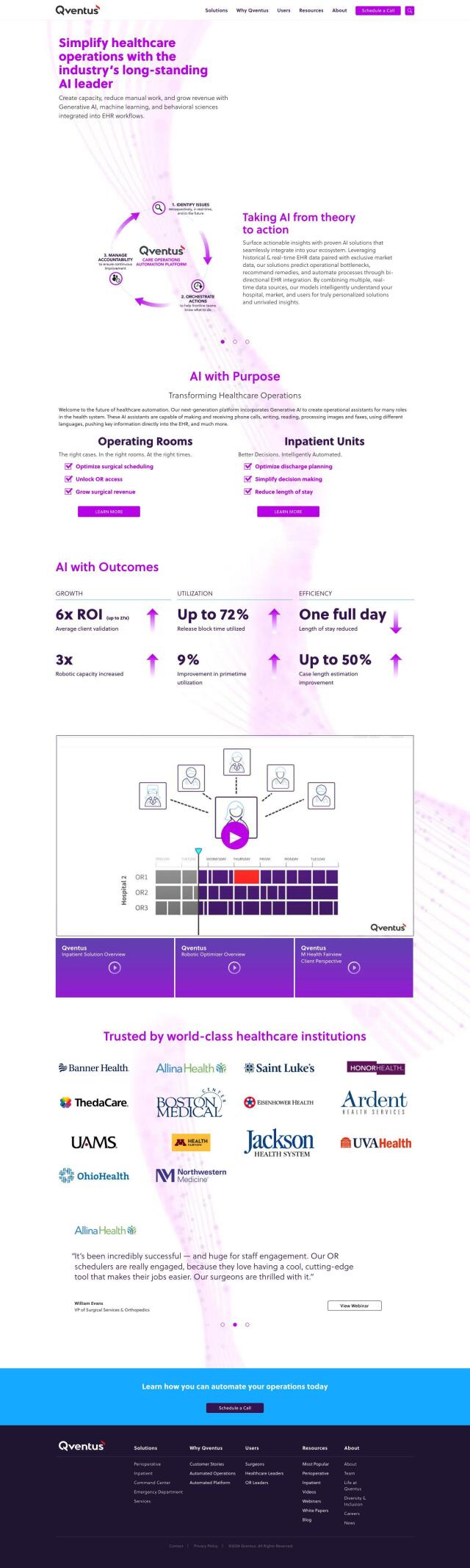
Qventus
If you want a more integrated approach, Qventus has a healthcare operations platform that uses AI, machine learning and behavioral science to optimize patient flow and operational performance. It integrates with EHR workflows to automate processes, forecast operational constraints and recommend solutions. By automating tasks like phone calls and document processing, Qventus can help reduce manual work and improve overall healthcare operations.
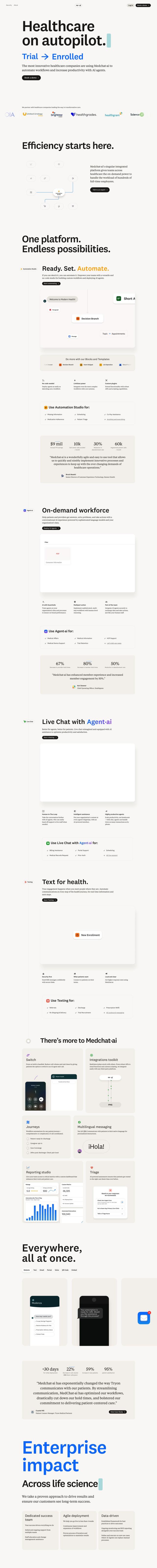
Medchat·ai
Also worth a look is Medchat·ai, an AI-powered automation platform designed to automate healthcare workflows and improve productivity. It includes tools like Agent·ai for conversational AI experiences, Live Chat for AI-assisted human support, and Texting for automated communications. Medchat·ai seeks to reduce provider hold times, member hold times and abandonment rates while improving patient engagement and satisfaction.