Question: I'm looking for a solution that automates prior authorizations and reduces delays to patient care.

Availity
If you're looking for ways to automate prior authorizations and cut delays in patient care, Availity is a broad option worth evaluating. Availity's integrated provider engagement platform uses AI to automate administrative and clinical tasks, including automated prior authorization processes. With features like revenue cycle management, eligibility and coverage solutions, and denial prevention tools, Availity can help healthcare providers deliver better patient care and run more efficiently.
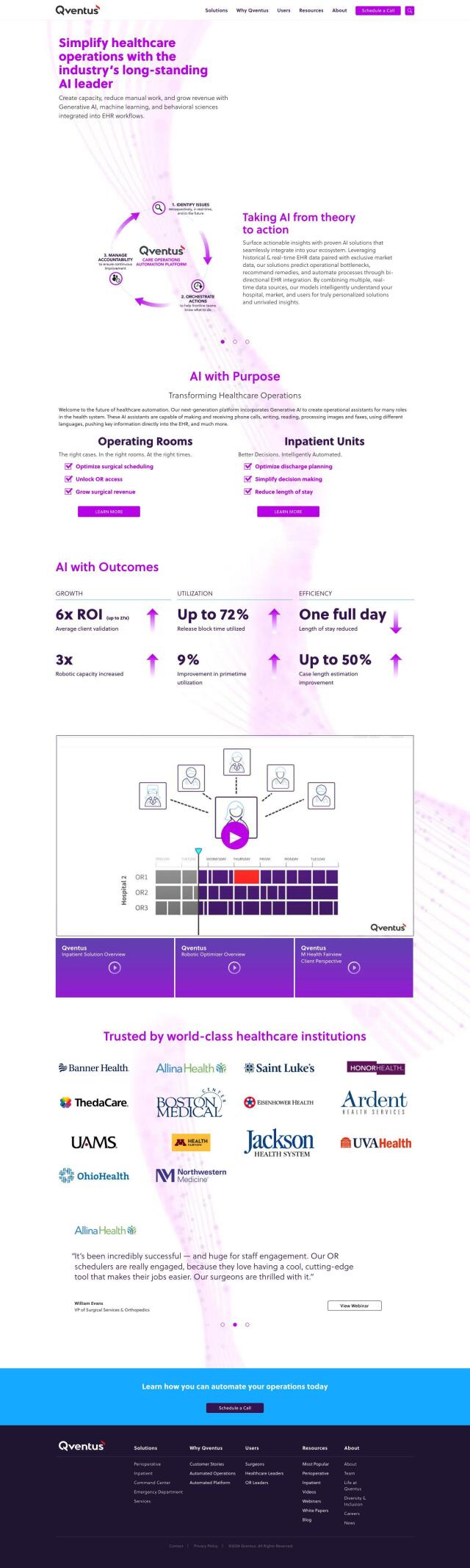
Qventus
Another option is Qventus. Qventus uses AI, machine learning and behavioral science to optimize healthcare operations, including patient flow and prior authorization. By automating tasks like phone calls and document processing, Qventus can cut manual labor and improve performance, which can help speed up patient care.
Athelas
If you want to improve your revenue cycle management, Athelas offers a range of AI-based tools. Its Athelas RCM module automates operations and offers real-time insights for better decision making. And Athelas Scribe and Patient Care modules automate transcription services and remote patient monitoring so healthcare providers can spend more time on patients and less on paperwork.
Abridge
Last, Abridge is worth a look. This generative AI platform converts clinical conversations into structured notes that can be integrated with Epic systems. Abridge eases documentation burdens so clinicians can save time and improve patient care quality. By freeing up clinicians from documentation, healthcare providers can spend more time with patients and improve patient care efficiency.