Question: Is there an EHR system that can accurately turn speech into clinical notes and help with documentation?
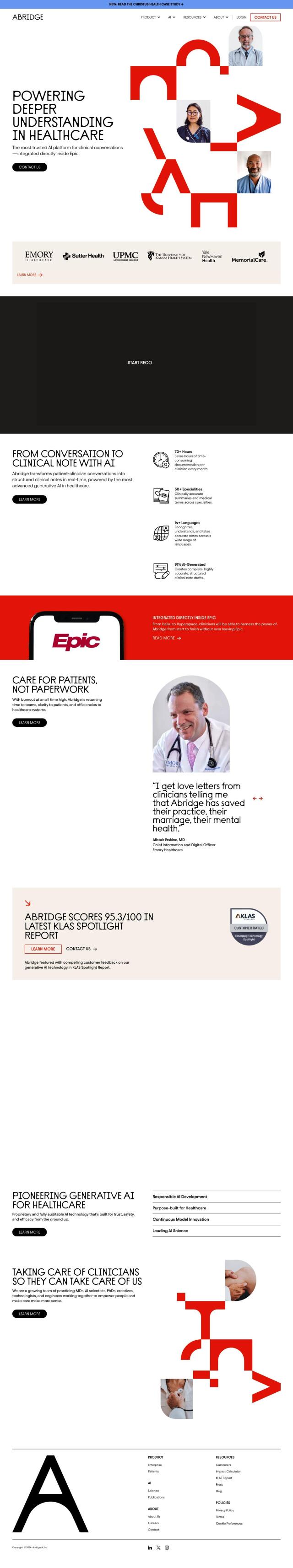
Abridge
If you're in the market for an EHR system that can transcribe speech into clinical notes to ease documentation, Abridge is worth a look. Abridge is a generative AI platform that turns clinical conversations into structured notes that are built directly into Epic systems. It can generate notes in real time, handle multiple languages, and provide verifiable notes that are checked against conversation transcripts and audio recordings. That can free clinicians from documentation work for as much as 70 hours a month and let them have a better work-life balance.
Suki
Another good option is Suki, an AI-powered voice assistant designed to automate clinical workflows. Suki can generate ambient notes, dictate text and suggest coding, and it integrates tightly with major EHR systems. It's secured with industry-leading tools and is HIPAA and SOC2 Type 2 compliant. Suki cuts documentation time by 72% and boosts physician satisfaction by letting clinicians spend more time on patients.
NextGen Healthcare
NextGen Healthcare also has a powerful option with its NextGen Ambient Assist feature, which transcribes patient-provider conversations into clinical notes and structured SOAP notes. That can free up providers to spend up to two hours a day on other work. NextGen Healthcare offers customizable clinical care workflows, patient engagement tools and specialty-specific options, so it's a good choice for practices large or small.
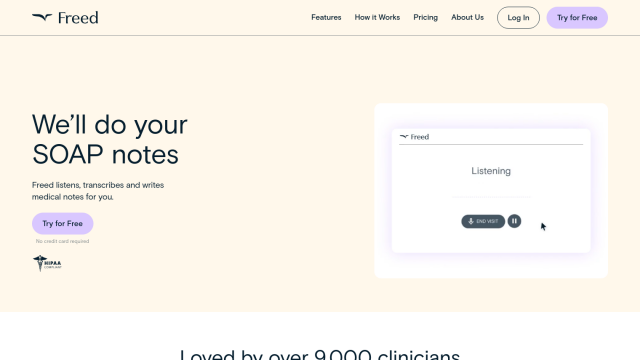
Freed
If you're looking for a medical scribe option, check out Freed. Freed learns a clinician's style and formatting to generate customized clinical notes in minutes. It can transcribe directly into EHR systems and can work even in noisy environments. Freed is HIPAA compliant and focused on cutting clinician documentation time, so it can help them spend more time with patients and less time worrying.