Question: Can you recommend a clinical documentation tool that integrates with existing workflows and meets Australian healthcare standards?
MedReport AI
If you're looking for a clinical documentation tool that fits into your existing workflow and satisfies Australian healthcare requirements, MedReport AI is a good choice. This tool is designed for mental health professionals in Australia and uses AI to generate detailed reports including Medicare updates, progress notes, discharge summaries and referrals. It can save up to 88% of documentation time and ensures compliance with Australian healthcare regulations and standards. With built-in access to DSM-5 and ICD-11 knowledge, it's designed to accommodate the subtleties of mental health documentation.
Abridge
Another top contender is Abridge, a generative AI platform that converts clinical conversations into structured notes. Abridge connects directly to Epic systems and offers real-time note generation, support for multiple languages, and verifiable notes validated against original conversation transcripts and audio recordings. It eases the documentation burden, freeing clinicians up to spend up to 70 hours a month on other tasks, and improves work-life balance. Abridge also satisfies HIPAA requirements and stores data in the cloud securely.
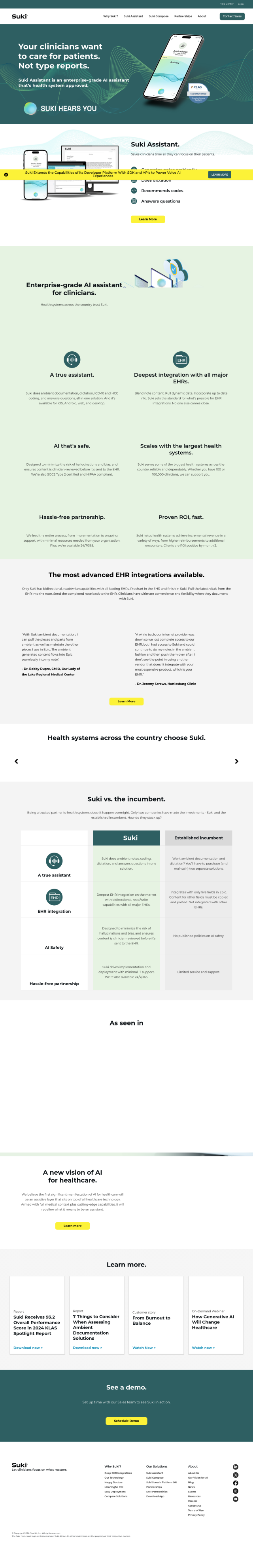
Suki
If you prefer a voice-activated documentation tool, Suki is worth a look. Suki is an AI-powered voice assistant that automates clinical workflows with features like ambient note generation, dictation, code suggestion and question answering. It connects deeply to big EHR systems like Epic, Cerner and Athena, so it fits right into your existing workflow. Suki complies with HIPAA and SOC2 Type 2 requirements for data security, and is designed to free up time for clinicians so they can spend more time on patient care.