Question: Do you know of a platform that offers customizable templates and smart phrases to simplify clinical documentation and reduce clinician burnout?
Suki
For a platform that provides customizable templates and smart phrases to ease clinical documentation and combat clinician burnout, Suki is a top contender. The AI-powered voice assistant automates administrative tasks like dictation, code completion and note writing for clinicians. Suki is deeply integrated with big EHR systems, offers read/write access, clinician-reviewed content and HIPAA and SOC2 compliance. It promises to cut documentation time by 72% and improve physician satisfaction and retention by avoiding burnout.
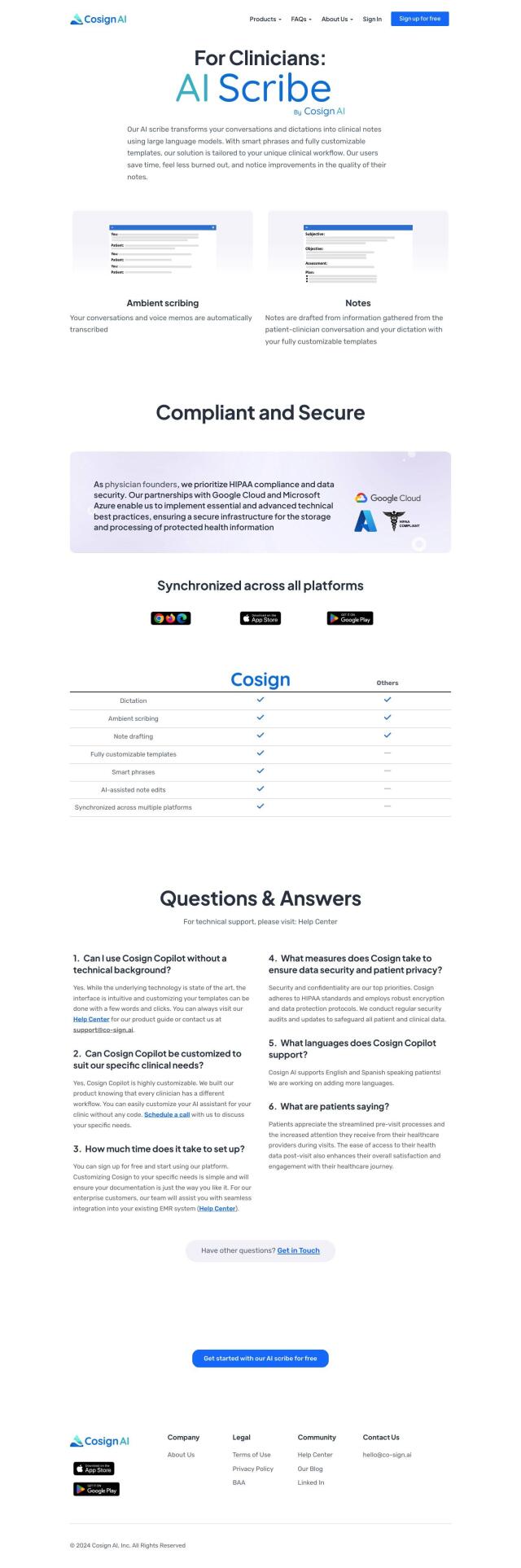
Cosign AI
Another top pick is Cosign AI, which uses AI tools to accelerate clinical documentation and other aspects of healthcare. It offers dictation, ambient scribing and note drafting abilities that turn clinician conversations into clinical notes with smart phrases and fully customizable templates. The platform is HIPAA compliant and offers synchronized access across multiple systems, making it easy to use and efficient.
Abridge
For an Epic integration and real-time note generation, Abridge is a top choice. The generative AI platform converts clinician conversations into structured notes, offering clinically validated summaries across 50+ specialties. It supports multiple languages and offers features like verifiable notes and enterprise solutions with custom governance controls, analytics and HIPAA compliance.
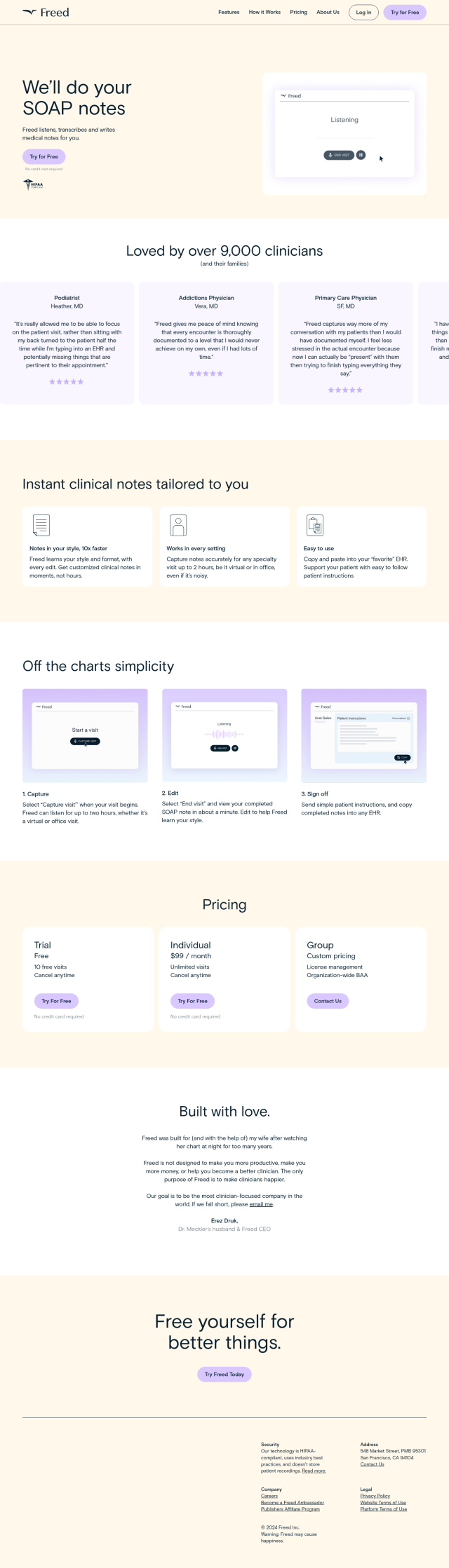
Freed
Last, Freed is an AI-powered medical scribe designed to help clinicians create customized clinical notes as fast as possible. It learns a clinician's style and formatting over time and integrates with EHR systems. Freed ensures accurate transcription and offers individual, group and enterprise plans, so it's adaptable for reducing documentation time and improving productivity.