Question: I'm looking for a tool that can automate progress notes and report writing for my healthcare team.
MedReport AI
If you're looking for a tool to automate progress notes and report writing for your healthcare team, MedReport AI is a highly recommended option. This clinical documentation tool is designed for mental health practitioners in Australia, leveraging AI to produce detailed reports, including Medicare updates, progress notes, discharge summaries, and referrals. It can save up to 88% of documentation time and is compliant with Australian healthcare regulations, making it an efficient and secure solution.
Abridge
Another excellent choice is Abridge, a generative AI platform that turns clinical conversations into structured notes directly integrated with Epic systems. Abridge offers real-time note generation, support for multiple languages, and verifiable notes validated against original conversation transcripts and audio recordings. This tool can save clinicians up to 70 hours per month, improving documentation efficiency and reducing burnout.
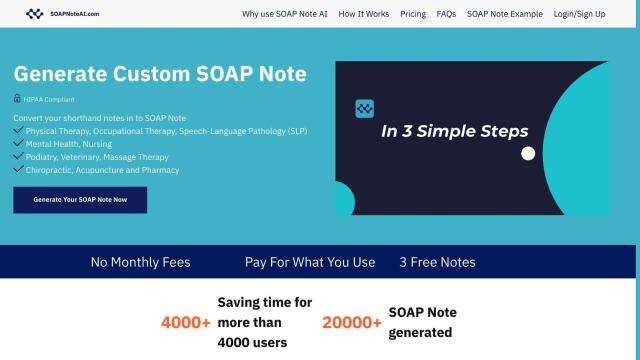
SOAP Note AI
For a more general-purpose AI assistant, consider SOAP Note AI. This HIPAA-compliant tool helps various healthcare professionals, including physical therapy and mental health, write SOAP notes and progress notes, cutting down daily documentation time by up to 50%. It supports multiple specialties and offers customizable SOAP notes to streamline documentation workflows.
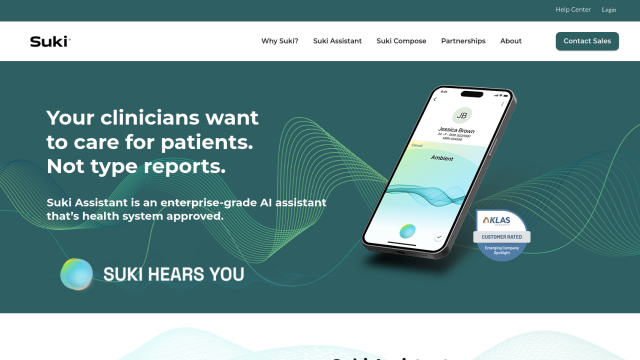
Suki
Lastly, Suki is an AI-powered voice assistant designed to automate clinical workflows, including note generation and dictation. It works across multiple specialties and integrates deeply with EHR systems like Epic and Cerner. Suki aims to reduce documentation time and improve physician satisfaction, making it a valuable tool to free clinicians from administrative tasks and focus on patient care.